[Updated: 2 August 2018] According to the US Centre for Disease Control (the CDC) more than 35% of US adults are obese and over 34% are overweight.[1] This weight issue is three times more common today than in the previous generation. Weight is clearly something that affects most of us but does fat or obesity cause migraine? Several scientific studies have looked at the interaction between obesity and migraine and found a relationship between them. [2] [3] [4] [5] More frequent and severe attacks are associated with people who are overweight. [2] [3] [4] [5]
Contents
The BMI weight standard
The body mass index (BMI) is the standard used to determine an individual’s weight-related health risk. It is a calculation of weight-to-height ratio. Based on height, the BMI provides a guide for an individual’s weight. They are considered guides as the BMI does not take into account muscle or bone mass or fat distribution around the body. A BMI index in people varies from 15 (borderline starvation) to over 40 (morbidly obese). Individuals are generally classified under the following categories:
Underweight: Under 18.5
Normal weight: 18.5-24.9
Overweight: 25-29.9
Obesity: 30-34.9
Morbidly Obese: 35 or more
To calculate your BMI. BMI = Weight(kg)/Height(m)2 Limitations of the BMI which mean it is less accurate in bodybuilders, weightlifters, high-performance athletes, pregnant women, the elderly or people under 18 years.
Waist Circumference is an Indicator of Disease Risk
Waist circumference is another important measure which compliments the BMI. Weight carried around the stomach is a greater health risk than weight on the hips or thighs. Weight circumference is also a better estimate of visceral fat, the type of fat which coats the organs and is more problematic. The waist circumference thresholds that indicate an increase of risk of disease are listed below by gender: For women:
- your risk is increased at 80 cm or more
- your risk is high at 88 cm or more
For men:
- your risk is increased at 94 cm or more
- your risk is high at 102 cm or more
To calculate your risk, click here to use this free online calculator. If your measurements indicate an increased risk it can directly contribute to the following:
- type 2 diabetes
- high blood pressure
- sleep apnea
- osteoarthritis
- cardiovascular risk
But what about headache and migraine?
GET A LIST OF NATURAL ALTERNATIVES PROVEN TO HELP MIGRAINE. FREE FOR A LIMITED TIME.
Migraine and Obesity
A recent 2017 peer-reviewed published study found a direct link in the reduction of excess weight with a significant reduction in migraine frequency. [4] Study participants were females with 4-20 migraine days per month with a BMI between 25 and 49.9. The study found that the average number of migraine days had fallen by almost half at the followup period. [4] What did they do? Participants received a 16-week behavioral weight loss program which included 3 components:
- A standard calorie and fat-restricted diet with goals of 1,200-1,500 calories per day and 33-42 grams of fat per day.
- A gradual progression up to a goal of 250 mins per week of moderate-intensity, home-based exercise (i.e. 50mins, 5 days per week).
- Behavioral modification strategies such as self-monitoring (diet, exercise, weight), goal setting, stimulus control and problem-solving to modify eating and physical activity.
A separate large population study found that obesity is associated with the frequency and severity of migraine attacks. The higher the weight and BMI group of the individual, the higher the attack frequency and severity. It did not find that obesity was a risk factor for developing the migraine disorder or disease. [2] In other words, being overweight or obese doesn’t cause migraine, but if you have migraine it can make it significantly worse. 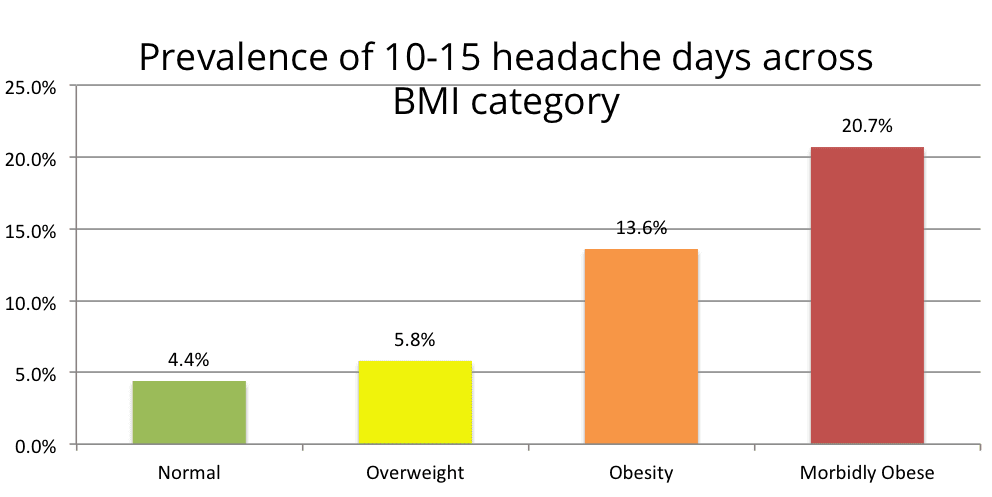 If you do have migraine and you’re overweight then the results suggest if you lower your weight to a normal BMI group or even one BMI group downward (eg. from obese to overweight) then the frequency and severity of your attacks is likely to improve as well.
If you do have migraine and you’re overweight then the results suggest if you lower your weight to a normal BMI group or even one BMI group downward (eg. from obese to overweight) then the frequency and severity of your attacks is likely to improve as well.
Chronic Daily Headache and Obesity Chronic daily headache (CDH) are headaches occurring on 15 or more days per month.[3] The most common types of CDH are transformed migraine and chronic tension-type headache. Transformed migraine occurs in those with migraine whose attacks increase in frequency. Chronic tension-type headache evolves from episodic tension-type headache. [3] A study looking at the factors associated with the onset and remission of CDH in a population found that obesity was associated with a five-fold increased risk of developing CDH.[5] A second study also found a clear relationship between the prevalence of chronic daily headache and transformed migraine according to BMI. 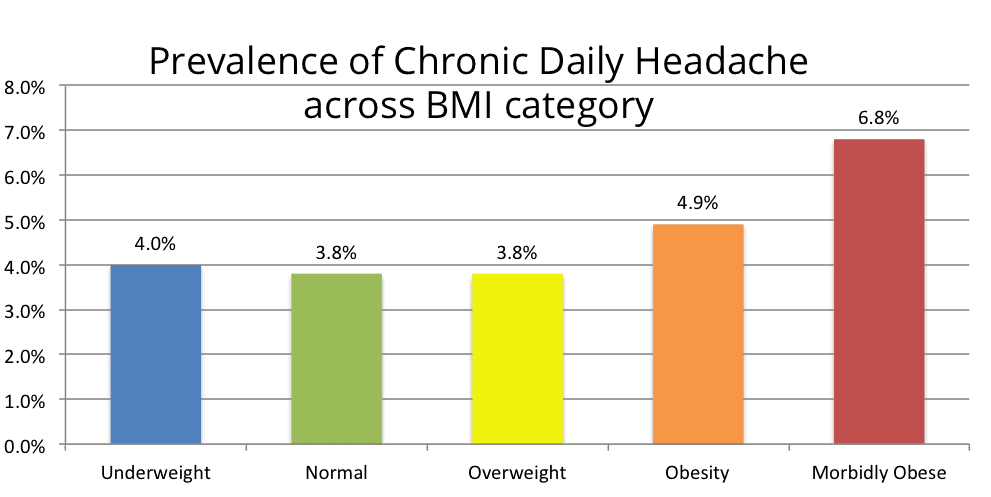 Below you can see how weight similarily influences the likelihood of Transformed Migraine as weight increases.
Below you can see how weight similarily influences the likelihood of Transformed Migraine as weight increases. 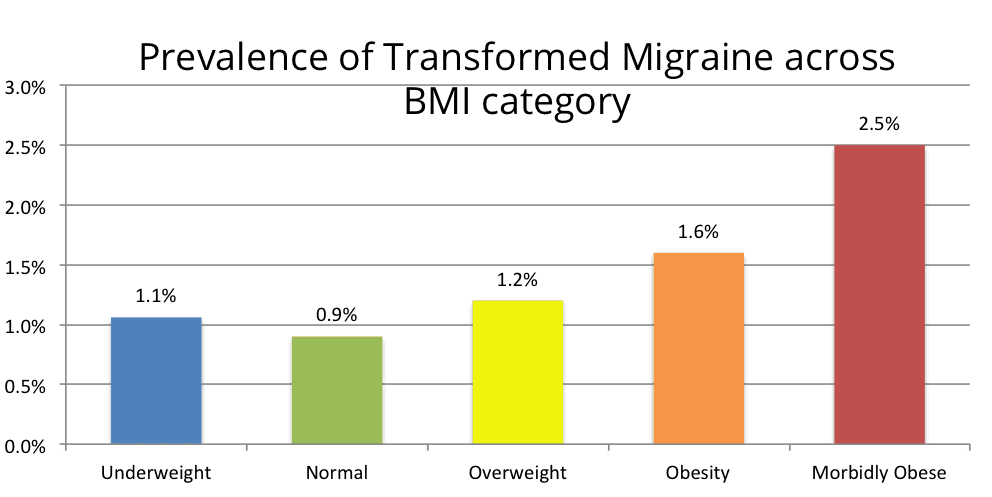
Both charts above show a clear trend indicating that the heavier the BMI weight category you fall into, the higher the likelihood of CDH and transformed migraine.
The trend in transformed migraine is significant. This trend was not found in chronic tension-type headache which was also evaluated in the same research study.
How Does Obesity Affects Migraine Frequency & Severity?
We know that obesity doesn’t cause migraine but it does correlate with the frequency and severity of attacks. How exactly? Researchers aren’t precisely sure, but there are several reasonable theories proposed:
1. Inflammation
The interrelationships between headache frequency and obesity are complex. Obesity itself is a pro-inflammatory state. Biomarkers of inflammation inside the body are elevated in those individuals who are obese. [6] There are several proposed mechanisms by which obesity may contribute to higher levels of inflammation. Inflammation is an important consideration for migraine which is associated with neurovascular inflammation. [7] Some experts may reason then that the more inflammation in someone with migraine the more likely frequent and/or more severe attacks.
2. CGRP
CGRP or calcitonin gene-related peptides are molecules that keep coming up in migraine discussions and treatments. CGRP is a neuropeptide which plays an important role in a migraine attack. CGRP itself is released during a migraine attack. Interestingly there are several potential links between this molecule, obesity, and migraine which suggest a relationship. [8] Studies have shown that levels of CGRP are elevated in obese individuals. Particularly in women. [9] This biological link hasn’t yet been fully studied so this still remains hypothetical, however, CGRP inhibitors have been shown to be effective in treating migraine. This suggests to researchers that CGRP may also be playing an extra important role in migraine and obesity.
3. Dietary choices
In some cases obesity may be due to a separate medical illness or as a side effect from commonly prescribed migraine medications. In other cases our weight is a reflection of our dietary habits, food choices, and lifestyle. Overweight individuals are more likely to consume higher levels of processed foods than those whose weight sits in the normal BMI range. Processed foods contain numerous amounts of excitotoxins, chemicals, and artificial ingredients which may contribute to inflammation and overstimulate the sensitized migraine brain. This could potentially contribute to more attacks. More scientific research is needed in this area before this can become more than a hypothesis but it could be a piece of the obesity and migraine puzzle. Read more about potential triggers here.
4. Exercise
At higher levels of the BMI, it becomes more difficult to exercise. Exercise is less about weight loss and more about fitness and strength. Even large amounts of regular exercise cannot offset a diet full of processed food, artificial preservatives, additives and sugar. Studies have shown that regular cardiovascular exercise can help protect against migraine and is as effective as a commonly prescribed migraine preventative Topiramate.[10] Despite the evidence, exercise may still represent a challenge for overweight patients with migraine. They may have exertional headache where a headache is triggered by extra effort or overheating. This can make regular cardio exercise more difficult to practice. For the majority of patients, regular exercise is great for brain health, sleep, stress and migraine prevention. If you are overweight and wish to begin exercising check first with your doctor and start small, then build up gradually. Despite best intentions, jogging 5 miles after an extended period of no exercise is a recipe for disaster.
Conclusion
Research mentioned in this article suggests that addressing obesity results in fewer and less severe attacks. This applies to both adults and children and for those with chronic or episodic migraine. Benefits can accrue from either weight loss from diet/exercise changes or from surgical weight loss procedures. Clinical trials with control groups and robust methodologies are still lacking for a definitive statement about obesity and migraine reduction however the link is clear. Have you had trouble losing weight whilst juggling migraine? Let me know in the comments.
Get a list of 11 natural and proven treatments from medically published studies sent to you.
Article References
[1] NIH Website ‘ Obesity and Overweight’ https://www.nichd.nih.gov/health/topics/obesity/conditioninfo/pages/risk.aspx Accessed 4 Dec 2017.
[2] Bigal, Marcelo E., Joshua N. Liberman, and Richard B. Lipton. “Obesity and migraine A population study.” Neurology 66.4 (2006): 545-550.
[3] Bigal, Marcelo E., and Richard B. Lipton. “Obesity is a risk factor for transformed migraine but not chronic tension-type headache.” Neurology 67.2 (2006): 252-257.
[4] Bond, Dale S., et al. “Behavioral Weight Loss Intervention for Migraine: A Randomized Controlled Trial.” Obesity 26.1 (2018): 81-87.
[5] Scher, A. I., et al. “Factors associated with the onset and remission of chronic daily headache in a population-based study.” Pain 106.1 (2003): 81-89.
[6] Lee, Yong-Ho, and Richard E. Pratley. “The evolving role of inflammation in obesity and the metabolic syndrome.” Current diabetes reports 5.1 (2005): 70-75.
[7] Bigal, Marcelo E., and Richard B. Lipton. “Obesity is a risk factor for transformed migraine but not chronic tension-type headache.” Neurology 67.2 (2006): 252-257.
[8] Recober, Ana, and Peter J. Goadsby. “Calcitonin gene-related peptide (CGRP): a molecular link between obesity and migraine?.” Drug news & perspectives 23.2 (2010): 112.
[9] Bigal, Marcelo E., and Richard B. Lipton. “Obesity is a risk factor for transformed migraine but not chronic tension-type headache.” Neurology 67.2 (2006): 252-257.
[10] Varkey, Emma, et al. “Exercise as migraine prophylaxis: a randomized study using relaxation and topiramate as controls.” Cephalalgia 31.14 (2011): 1428-1438.
Chronic Migraine is what caused me to be overweight, not the other way around. I was just as chronic when I was 120 lbs. (5’4") as I am at 160 lbs., which is weight that got put on when my migraine gained the symptom of diarrhea. Actually, I was up to 170 lbs., but lost 10 lbs. when I was on topiramate for six months (had to stop it due to an allergy, but it was helpful with preventing the migraines – not sure if the loss was from the med or from no longer having the diarrhea because of no more migraines). I don’t have food triggers. I can’t exercise because of the vertigo from the migraines. It sucks, as does everything else to do with migraine!
It can be a vicious cycle that feeds on itself. Migraine makes it difficult, painful and sometimes impossible to exercise. This can lead to weight gain. Excess weight can propagate further inflammatory processes in the body and worsen migraine.
Makes sense. I’m so glad they’ve come out with this study. Obesity is an epidemic and it puts the control back in the hands of the people. You have the power to change!
We can control some of the risk factors, but sometimes it is easier said than done. I hope this provides some inspiration for you Brynn.
This study which didn’t mention estrogen dominance which is a big problem in the western world and its from plastics and other things as plastic has a estrogen effect in our bodys in other words plastics mimic estrogen in our bodies ,when we drink from plastic bottles and a lot of other things and estrogen dominance can cause hormonal migraines, we cannot escape this plastic estrogen problem as we are swimming in plastics so what are we meant to do, most people haven’t the time to cut out all plastics and I doubt that is even possible if we live in the western world!!!
Marty, the natural fluctuation in hormones in a healthy female is enough to trigger migraine. Estrogen imbalance is not a prerequisite but it may also be a contributing factor. For more on this subject see this article: https://migrainepal.com/prevent-menstrual-migraine/
I completely identify with this research. Although the migraines & CDH began long before I was overweight, the heavier I have gotten the worse the headaches. My main trigger is processed foods. Staying away from those reduces migraine from 4-5 a week to 1 a week. This diet change has also reduced my weight by 20 lbs, slowly. I have also discovered migraine is worse if I do not stay hydrated, with water.
My problem continues to be one mentioned in the article, exertion migraine. What to do about that? Walking more than 10 min will trigger. So frustrating!
Congratulations on that progress. That is a fantastic achievement Cathy. Even though you still feel frustrated, recognize the massive improvement up to an 80% reduction that you have achieved.
To go further and to be able to exercise, it may mean working in partnership with your doctor to gradually build up and also uncover what is still playing a role in sensitizing or causing an overreaction from the nervous system these may be other triggers. You may find that a preventative treatment may help just before you plan to exercise. Hopefully your doctor will have some suggestions for you personally.
Take care.
Absolutely agree. Same story. 130 lbs. chronic migraine 20 years, 200lbs! I can do yoga once a week and most days an hr walk. Still lbs keeping coming?
The harsh reality is diet is the biggest factor versus how much we exercise. Exercise is still extremely important for migraine, general health and longevity, but it is perhaps 20% whereas the other 80% is diet when it comes to weight gain….
The other factor not taken into consideration is medication and side effects. These can play havoc with weight and are different for everyone.
I have found it impossible to lose weight with chronic migraine. Hunger produces a headache which quickly becomes migraine. Exercise produces migraine, even moderate exercise. It feels hopeless, even though I am on an antidepressant. That’s another thing- I am on so many meds to either prevent or treat migraines they interfere with exercise and willpower as well as good judgement.
Hi Karen,
I’ve had hunger trigger a migraine when I was trying intermittent fasting (and really feeling great otherwise). It was very frustrating as I was doing so well. It is SO difficult at times. That’s why it’s really important in my experience to a) have some you can talk to about it… preferably another migraine patient where you can share experiences and b) work in partnership with a doctor who genuinely cares about your progress.
I struggle with obesity, in part because I take Depakote and the antihistamine Atarax to prevent migraine. They help tremendously, but one of the side effects is weight gain. I exercise 5-7 days/week (walking dogs), but find it hard to increase my level, as I also have Fibromyalgia.
(Can’t someone come up with a little magic pill that solves every health problem?! 😉)
Lol. That would be lovely, I feel like we spend enough on treatments and vitamins there should be something of that nature by now 😉 I can’t even imagine how much more difficult exercise would be with Fibromyalgia.
I was 120-135lbs until I started getting regular headaches & migraine, I’m 5’8 and 195lbs now (my heaviest ever)! Mine too get worse with exertion kinda difficult to raise 2 kiddos keep a house, keep a husband (sex is problematic) and keep friends. I’m lucky my mil lives with us! She pretty much does all the cooking, which is wonderful but she’s very overweight & makes a ton of prepackaged high fat, sugar & processed foods. With that and lack of exercise it feels like I’m stuck like this is it & this has are never going to change or get better.
Hi Tabitha, a little bit of education and changing of the diet can go a long way. You might be surprised just how much of an impact food has on our own health, not just weight but migraine severity and frequency too.
I certainly have struggled to keep my weight down as well as struggling with migraine.
I have not had migraine since iv been on either amlodopine for high blood pressure or, recently, Naproxin an anti inflammatory.
I have the apparent signs of rheumatism but no biomarkers according to my blood tests.
Migraine and weight has been my problem most of my life, especially since a teen.
Do you want to know more because I am happy to share more?
Kay Harding
Hi Kay, we are keeping track of remission examples here. Please do share here if you are willing: https://migrainepal.com/casestudies/
Thanks so much!
Sorry. Not sure if theres a connection between my migraines and overweight though it does make sense. Theres bound to be more stress for the overweight.
We never feel quite good enough and can find it harder than average to be accepted. Then if tragedy has hit ones life at some point its likely to add to the stress.
Hi Kay, no need to apologize. These studies didn’t find a 100% correlation which means there are always going to be exceptions. I think you’re right regarding stress and tragedy. Both are hugely significant and commonly accompany migraine.
I can relate to this as well. Physical exertion leads to immediate migraine. My vertigo, dizzy spells are something I cannot control. How do I tackle the weight gain from the steroids I’m on? What suggestions do you have when you are diagnosed with depression from your chronic illness?
Jessica having depression because you have awfully painful, frustrating and disruptive migraine attacks is a perfectly acceptable and normal human response. I had it. It took me a while to realize I didn’t need to feel shame about it. Often the depression goes away as the migraine condition improves (for obvious reasons) which also happened with me.
Regarding the weight gain this really comes down to a discussion between you and your doctor. If the treatment is working well, then it may be the lesser of two evils. If it isn’t, then it may be time to try something else.
I think the research needs to come a long way before identifying causation vs correlation. What if migraine-sourced increases in CGRP lead to subsequent weight gain response (further elevation in CGRP)? And if weight gain occurs over time, might other health changes account for the uptick in migraine – such as hormonal changes, worsening neuralgia?
The uptick in mine is due to a worsening in the cervical spine now impinging occipital nerves. I’m glad my doc didn’t just chalk it up to weight but ordered the MRI necessary to confirm.
The tendency to reduce significant health challenges to a simplistic mantra of "lose weight & exercise" is increasingly troublesome. I recall the story of a woman in the UK who died bc the doctors dismissed her, chalked her complaints up to weight, and totally missed the cancer that ultimately killed her. Weight bias can be a serious barrier to care and fodder for cruelty and prejudice. I think reporting on this issue should take that into account.
Also, I think migraine research and result analysis continues to be hampered by subjective identification of study populations. In cancer research, I think it’s unlikely that findings related to Stage 1 cancer would be generalized & applied to other Stages of cancer without serious consideration of the differences in populations. I’ve met "migraine sufferers" reporting significant impairment but with limited symptom sets and their activities are relatively unaffected. I respect their story, but that experience is not reflective of mine (or of others even more severely affected). It would be nice to know how appropriate (or not) it is to apply findings across this spectrum.
As for the question, yes, migraine & my other forms of headache (which also increase migraine frequency) do interfere with exercise. Dizziness and issues with proprioception – not to mention vomit-inducing pain with movement – come to mind as reasons why. I would be curious to know if Feldenkrais or Alexander techniques might be used to adapt some kind of migraine-friendly approach. Of course, migraine isn’t my only health challenge and the majority of exercise limitation (and lousy nutrition) comes from that. I’d love to be able to access a saltwater pool – asthma dictates no chlorine (as would migraine, come to think of it!)
Hi Cerys,
Your right, it’s not causation, it’s correlation. I’ve updated the offending sentence and replaced with correlate rather than contribute i.e. "…obesity doesn’t cause migraine but it does correlate with the frequency and severity of attacks." Thank you for your comment.
This surprises me.
I started migraines in the early 1980s so about 1984, At that time i needed to lose weight and get fit. Ergodryl was available and this is what i took to abort migraines when i could.
In 1987 I married and went to Australia. I became very fit through frequent swimming, cycling about often, hillwalking every 3-4 weeks. I was quite strong. I also took part in some karate classes. I could hang by the hand on a swing bar and pull myself up so i balanced on the bar by my hands. People sometimes saw me and praised and were surprised by me.
I had some bad mifgraines in those years with an outdoor life in Australia.
Coming back to the UK i had less chance, both geographically and financially, to take part in these activities. Migraines continued but I found Triptans and discovered one which worked for me. Nowadays I have problems with migraine aura. Also i am on meds for other problems and these seem to have an effect on my migraines. While I have migraine aura i have not had a full migraine for years. I am heavier than I have been since my days overseas !
So while i would like to get ontop of my weight problem I dont have true migraines.
Migraines could return anytime however and that is always a worry as is the problem of finding friends and employers who understand the problems I have. That is all stressfull Only a migraineur would understand this which is part of the stigma of living with migraine.
Stigma is harmful in any way its looked at.
It seems to me that the stress and lack of understanding a migraineur gets may cause many migraines.
I am pleased with the work many are doing to learm about migraine but I am disappointed it all comes back to being considered to be about diet and exercise again,
kay
That is a dangerous conclusion to draw. Saying migraine is entirely from obesity is not true. What we are seeing in the evidence are correlations. Not causations. Migraine is a multi-factorial chronic disease for many people. This is just one piece of a larger puzzle. It’s another factor to consider and another reason to ensure we are leading healthy lifestyles for those that might need one. I hope that helps Kay.
I seem to be in the midst of this issue now…gaining weigh almost daily with menstrual migraines. IT is so very frustrating. I;ll have an attack, that lasts days, it seems, and can barely take care of my children, let alone feed myself well. Then when I start to feel in control again, I get another attack. Do you find any one type of eating best? My genes say I should be on a low carb diet. I am wondering if keto would be best, or is it too drastic for migraine sufferers? Has there been any studies? Thanks for your time.
Hi Sara, there is another article on the website all about this topic of diet which you can find here I hope that provides some answers for you.
Very nice point, obesity causes a lot of problems
Glad you found this helpful. It is easy to blame something and losing weight is more difficult for some people than others. But it’s our health.